Regenerative Medicine Options: PRP vs Stem Cells
You've heard about regenerative medicine. You know it's supposed to help your body heal damaged tissue, reduce chronic pain, and potentially help you avoid surgery.
But then you start looking into it, and suddenly you're drowning in options.
PRP. Stem cells. Prolotherapy. Exosomes. Peptides.
Everyone's throwing around acronyms and technical terms, and you're just sitting there thinking, "I just want to stop hurting. Which one do I need?"
Here's the reality: not all regenerative medicine treatments are the same. They use different mechanisms, target different problems, and produce different results.
The two most common options you'll hear about are PRP (platelet-rich plasma) therapy and stem cell therapy. Both are powerful. Both can produce incredible results. But they work in fundamentally different ways.
Understanding the difference isn't just about being informed. It's about making sure you're choosing the treatment that actually matches what your body needs.
So let's break it down. No medical jargon. No sales pitch. Just straight talk about what these treatments do, how they work, and when each one makes sense.
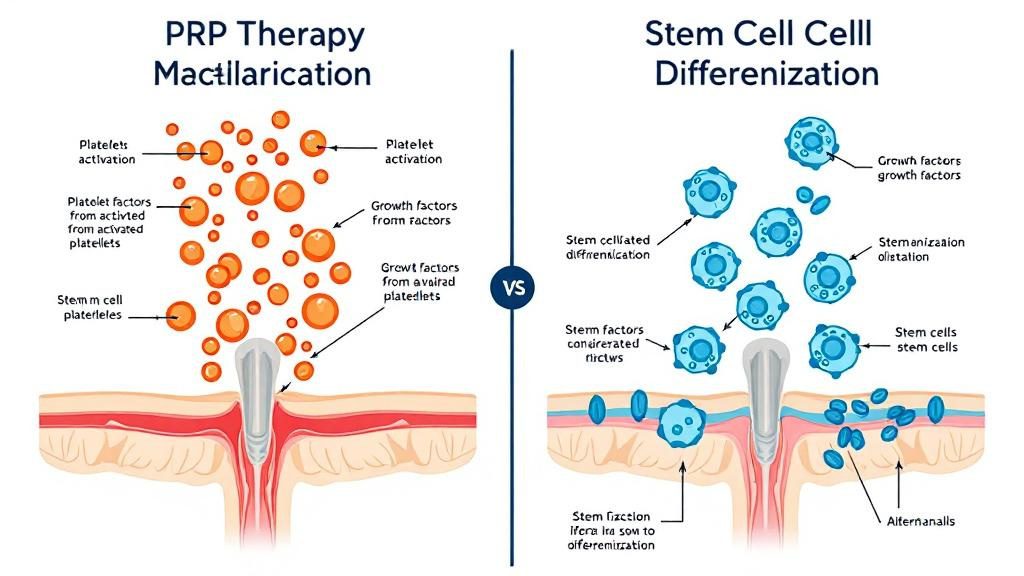
What Is PRP Therapy?

PRP stands for platelet-rich plasma. It's one of the most widely used regenerative medicine treatments, and for good reason: it works.
Here's how it goes down.
Your blood contains platelets—tiny cells that rush to injury sites and kickstart the healing process. When you cut yourself, platelets are what stop the bleeding and trigger tissue repair.
But platelets do more than just clot blood. They're loaded with growth factors, proteins that tell your body to rebuild damaged tissue, reduce inflammation, and accelerate healing.
PRP therapy takes your own blood, spins it in a centrifuge to concentrate the platelets, and injects that concentrated solution directly into injured or damaged tissue.
The result? You're delivering a massive dose of healing signals right where your body needs them most.
Your body recognizes the concentrated platelets, interprets it as a significant injury that needs attention, and ramps up the repair process. Inflammation decreases. Blood flow increases. New tissue starts forming.
It's not a foreign substance. It's not a drug. It's just your own biology, amplified and strategically deployed.
How PRP Is Harvested and Prepared
The process is straightforward.
A provider draws a small amount of your blood—usually about the same amount as a standard blood test. That blood goes into a centrifuge, which spins at high speed to separate the different components.
Red blood cells sink to the bottom. Plasma rises to the top. And right in the middle? That's where the platelets concentrate.
The provider extracts that platelet-rich layer, which now contains 5-10 times more platelets than your normal blood. That concentrated solution is what gets injected into your injured tissue.
The entire process takes about 30-45 minutes. Blood draw, centrifuge, injection. Same-day treatment with minimal downtime.
Because it's your own blood, there's virtually no risk of rejection or allergic reaction. Your body recognizes the platelets as its own and immediately puts them to work.
What Conditions Respond Best to PRP
PRP isn't a cure-all, but it's incredibly effective for certain types of injuries and conditions.
Tendon injuries respond particularly well. Tennis elbow, Achilles tendonitis, rotator cuff damage—tendons heal slowly on their own because they don't get much blood flow. PRP delivers concentrated healing factors directly to the site, speeding up repair.
Ligament sprains that won't fully heal are another strong candidate. If you've sprained an ankle or knee and it still feels unstable months later, PRP can help strengthen the damaged ligament tissue.
Osteoarthritis in its early to moderate stages benefits from PRP. It won't regenerate cartilage that's completely gone, but it can slow degeneration, reduce inflammation, and improve joint function.
Muscle injuries that aren't healing properly can also respond well, especially in athletes or active people who need to get back to performance quickly.
The common thread? PRP works best when your body is trying to heal but needs extra support to finish the job. It accelerates and enhances healing that's already happening—it doesn't create healing from nothing.
What Is Stem Cell Therapy?

Stem cell therapy takes regenerative medicine a step further.
If PRP is about accelerating your body's existing healing process, stem cells are about rebuilding tissue that your body can't repair on its own.
Here's what makes stem cells different.
Stem cells are undifferentiated cells—they haven't decided what they're going to be yet. When they're placed in damaged tissue, they read the environment and transform into whatever cell type is needed. Cartilage. Tendon. Ligament. Muscle.
It's like having a construction crew that can do any job. Need a carpenter? They become carpenters. Need an electrician? They become electricians. Stem cells adapt to what your body needs in that specific location.
This makes stem cell therapy incredibly powerful for conditions where tissue has been destroyed or severely degraded. We're not just talking about accelerating repair—we're talking about regenerating tissue that would never come back on its own.
Where Stem Cells Come From
There are several sources for stem cells, and the source matters.
Bone marrow-derived stem cells are harvested from your own body, usually from the hip bone. This is an autologous treatment, meaning it's your cells going back into your body. The procedure is more invasive than PRP—it requires a needle extraction from the bone—but the cells are proven and effective.
Adipose-derived stem cells come from fat tissue, usually harvested through a small liposuction procedure. These cells are easier to obtain in large quantities and still highly effective.
Umbilical cord-derived stem cells come from donated umbilical cord tissue after healthy births. These are allogeneic cells, meaning they're from a donor, not from your own body. They're younger, more potent, and don't require an invasive harvesting procedure on you.
Amniotic-derived stem cells come from amniotic fluid or membrane. Like umbilical cord cells, these are allogeneic and come from screened, healthy donors.
Each source has advantages and trade-offs. Autologous cells (from your own body) eliminate any risk of rejection but require a more invasive harvest. Allogeneic cells (from donors) are less invasive to obtain but require rigorous screening to ensure safety.
The key is working with a provider who uses properly sourced, tested, and regulated stem cell products. This isn't an area where you want to cut corners.
How Stem Cells Repair Tissue
Once stem cells are injected into damaged tissue, they get to work in multiple ways.
First, they directly differentiate into the tissue type that's needed. If you inject them into a damaged knee joint, they can become new cartilage cells and start rebuilding what's been lost.
Second, they release growth factors and signaling molecules that recruit your body's own repair cells to the area. They're not just repairing tissue themselves—they're telling your body to send reinforcements.
Third, they modulate inflammation. Chronic inflammation is one of the biggest barriers to healing. Stem cells help dial down the inflammatory response so your body can shift from damage mode to repair mode.
The result is tissue regeneration that wouldn't happen otherwise. Not just faster healing—actual rebuilding of structures that were beyond your body's natural repair capacity.
This is why stem cell therapy is often used for severe arthritis, major cartilage damage, and chronic degenerative conditions where PRP alone wouldn't be enough.
PRP vs Stem Cells: What's the Real Difference?
So which one is better?
That's the wrong question.
PRP and stem cells aren't competing treatments. They're complementary tools with different jobs.
Think of PRP as the repair crew. It shows up, accelerates the work that's already in progress, and helps your body finish what it started. It's highly effective for injuries that are healing but need a boost to complete the process.
Stem cells are the reconstruction crew. They show up when tissue is too damaged for your body to repair on its own, and they rebuild from scratch. They're for situations where your natural healing capacity has been overwhelmed.
Here's a simple way to think about it:
If your body is trying to heal but struggling, PRP gives it the resources to succeed.
If your body has stopped trying to heal because the damage is too severe, stem cells restart the process and regenerate tissue that would never come back naturally.
When PRP Makes More Sense
PRP is usually the first option to consider for most injuries and chronic pain conditions.
It's less invasive, less expensive, and highly effective for a wide range of problems. If you're dealing with tendonitis, ligament sprains, early-stage arthritis, or muscle injuries that won't heal, PRP is often all you need.
PRP works best when:
- Tissue is damaged but not destroyed
- Your body is showing signs of healing but hitting a plateau
- You need faster recovery from a sports injury or overuse condition
- You want a less aggressive option before considering stem cells
- Cost is a concern (PRP is typically more affordable)
Many people see significant improvement with PRP alone. If one treatment doesn't fully resolve the issue, multiple PRP sessions can be done to continue supporting the healing process.
When Stem Cells Make More Sense
Stem cell therapy is the choice when damage is severe or regeneration is needed.
If cartilage is significantly degraded, if ligaments are torn beyond what PRP can repair, or if you're dealing with advanced arthritis, stem cells offer a level of regeneration that PRP can't match.
Stem cells work best when:
- Tissue has been destroyed, not just damaged
- You're dealing with advanced arthritis or degenerative joint disease
- PRP has been tried and didn't produce sufficient results
- You're facing surgery and want one more non-surgical option
- You need actual tissue regeneration, not just accelerated healing
Stem cell therapy is more expensive and more complex, but for the right situation, it can be life-changing. It's not uncommon for people to avoid joint replacement surgery entirely because stem cells regenerated enough tissue to restore function.
Can You Combine PRP and Stem Cell Therapy?
Short answer? Yes. And in many cases, combining them produces better results than either treatment alone.
Here's why that works.
Stem cells are powerful regenerators, but they need the right environment to thrive. If the tissue is inflamed, damaged, and hostile, stem cells struggle to do their job.
PRP prepares the environment. It reduces inflammation, increases blood flow, and creates a healing-friendly environment where stem cells can function optimally.
Some providers use PRP as a first treatment to clean up the inflammatory mess and kickstart healing. Then, a few weeks later, they follow up with stem cell therapy to rebuild tissue that PRP couldn't fully restore.
Other providers inject PRP and stem cells together in the same session. The PRP creates the healing environment, and the stem cells immediately start regenerating tissue in that optimized space.
It's not always necessary to combine them, but for complex or severe conditions, the combination can be incredibly effective.
Sequencing Treatments for Best Results
The order matters.
If you start with PRP and see significant improvement, you might not need stem cells at all. Many people get everything they need from PRP alone.
If PRP helps but doesn't fully resolve the issue, stem cell therapy becomes the logical next step. You've already reduced inflammation and started the healing process—now you're adding the regenerative power to finish the job.
Starting with stem cells without addressing inflammation first is like trying to plant seeds in bad soil. The cells might not take hold as effectively as they would in a properly prepared environment.
This is why working with an experienced regenerative medicine provider matters. They understand how to sequence treatments, when to combine therapies, and how to adjust the approach based on your body's response.
Which Option Is Right for You?

The honest answer? It depends on what's actually wrong with your body.
PRP and stem cell therapy aren't interchangeable. They're targeted tools for specific problems. Choosing the right one starts with understanding the nature and severity of your injury or condition.
If you're dealing with chronic tendonitis, a ligament sprain that won't heal, or early-stage arthritis, PRP is probably your best starting point. It's effective, affordable, and minimally invasive.
If you're dealing with severe cartilage loss, advanced arthritis, or tissue damage that's beyond what your body can naturally repair, stem cell therapy might be the better option.
The best approach? Talk to someone who specializes in regenerative medicine. Not someone who only offers one type of treatment and pushes it regardless of your situation. You want a provider who can assess your specific condition and recommend the treatment that actually matches your needs.
Regen and Restore offers both PRP and stem cell therapies and works with patients to determine the best approach for their situation. Because they're in the same building as Atlas Chiropractic, your care stays coordinated—your chiropractic progress informs your regenerative treatment plan, and vice versa.
You can learn more about their approach and treatment options at regenandrestore.me.
Questions to Ask Before Starting Treatment
Before you commit to any regenerative medicine treatment, make sure you're asking the right questions.
What's the source of the cells or platelets? If it's stem cells, where do they come from? If it's PRP, how is it prepared and concentrated?
How many treatments will I need? Some conditions respond to a single session. Others require multiple treatments over several months.
What's the expected timeline for results? PRP typically shows improvement within 4-6 weeks. Stem cells can take 2-3 months to fully integrate and show results.
What happens if the first treatment doesn't work? Is there a follow-up plan? Can treatments be adjusted based on your response?
What are the risks and side effects? Both PRP and stem cells are generally safe, but every medical procedure carries some level of risk. Make sure you understand what to expect.
How much does it cost, and is it covered by insurance? Regenerative medicine is usually not covered by insurance, so you need to know the financial commitment upfront.
The more informed you are, the better decisions you'll make about your care.
The Bottom Line on PRP vs Stem Cells

Regenerative medicine isn't a magic bullet, but it's a legitimate option for people who need more than conservative care but want to avoid surgery.
PRP therapy accelerates healing in damaged tissue. It's effective, minimally invasive, and works for a wide range of injuries and chronic conditions.
Stem cell therapy regenerates tissue that your body can't repair on its own. It's more complex, more expensive, but potentially life-changing for severe damage and degeneration.
Neither one is universally better. They're different tools for different problems.
The key is matching the treatment to your specific condition, working with a provider who understands both options, and making sure your care is coordinated with the rest of your healthcare team.
If you've been dealing with chronic pain, old injuries that won't heal, or degeneration that's limiting your life, regenerative medicine might be exactly what your body's been waiting for.
And if you're already under chiropractic care at Atlas Chiropractic, the fact that Regen and Restore is in the same building means your treatment plan stays seamless. No conflicting advice. No bouncing between providers who don't communicate.
Just comprehensive care designed to get you back to living without limits.
Want to explore your options? Check out Regen and Restore and see what's possible when your body gets the support it actually needs.
Recent Blog Posts...
How Long Does Regenerative Medicine Take to Work?
Regenerative Medicine: A New Approach to Chronic Pain
Regenerative Medicine Options: PRP vs Stem Cells
When to Consider Regenerative Medicine Treatment
Living With Pain
Care of Concussions
Office Hours
2:00 PM - 5:30 PM
2:00 PM - 5:30 PM
Office Hours
2:00 PM - 5:30 PM
2:00 PM - 5:30 PM
Copyright 2026 | Atlas Chiropractic | All Rights Reserved | Website by iTech Valet






